CVS Caremark Reviews Summary
CVS Caremark has a rating of 1.1 stars from 228 reviews, indicating that most customers are generally dissatisfied with their purchases. Reviewers dissatisfied with CVS Caremark most frequently mention customer service, mail order and prior authorization. CVS Caremark ranks 8th among Pharmacy sites.
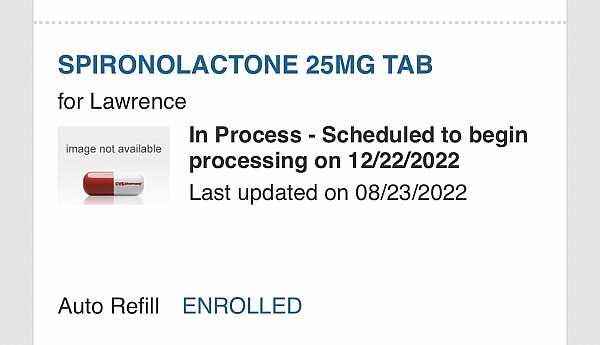
I asked my provider to send the prescription to this company based on the prices. In every other pharmacy situation, including mail order that I have used in the past, the patient/customer has to then call or click a text box asking that the pharmacy FILL the prescription. This allows the customer to double check the medication, the dose, and cost and decide if the drug at CVS Caremark is what they want to purchase. INSTEAD, I got medication in the mail without agreeing to the prices, amounts, etc! I have a bill for the medication which I was waiting for lab results to choose to fill or not! This is ridiculous and I am SHOCKED! It's like being in a hospital where the doctor orders a med and you get the bill later without being able to shop or consent. There is no patient request or consent! Instead they fill it and bill you. Beware!
Caremark mail order service is pathetic. They allows me to run out of Crohn's meds, twice, the last time for ten days. It is impossible to speak with a human and took an act of Congress to opt out of their services. I wouldn't use them again and I certainly would never recommend them.

My wife and I have medicare part D with this company. They are awful to deal with. The drugs we use are on their formulary, but they put you through hell to get them filled. They say that they require pre-approval. I have had other part D plans with different companies in the past and have never had this much difficulty in dealing with a company. I will not renew with them next year and would NOT recommend them to anyone. THEY ARE AWFUL!

I really like Cigna but they switched their prescription approvals to CVS Caremark and now the the service is horrible it is interesting how a company can subcontract their management to another company like Cigna did and ruin the great service they were providing I wonder if Cigna cared about the poor service

Please read my entire review I'm all about the fact's.
Henkel US, or Aetna Insurance decided to switch my prescription coverage to Caremark. I have the usual problems (screwed up prescriptions, auto text messages saying I'm covered/not covered on the same day, filled prescriptions/not filled when I pick them up, etc) with my prescriptions that everyone has until last week. I'm 58 years old have auto immune disease, osteoarthritis, now degenerative disk disease that over the past few years has caused me to be on more medications 9 to be exact. I'm now able to control my pain and function as a normal person. I put weight on the most in my lifetime. I stopped drinking, I walk 3-4 times a week, I changed my diet, I lost 12 of the 70 lbs put on. My Doctor decided after a year of me working on myself to help because I'm now borderline diabetic and my cholesterol is getting to the point of medication, More Prescriptions. She prescribed weight loss medication. Denied. I was told to have my doctor file an urgent appeal so it would go through. Denied. I was told to call Henkel US Benefits Customer Service. The Benefits service representative transferred me back to Caremark. Another Caremark representative stated ALL weight loss medication is NOT COVERED. Final answer Caremark does Not Cover Any Weight Loss Medication, Zero.
I asked the representative why I had to take Numerous Medications to not have a stroke or heart attack or become a diabetic when ONE Weight loss medication could prevent it and possibly stop my blood pressure and some pain medication. I informed him that all the Weight Loss medicine is temporary (some are 3 months, some 6 months) that the medications available state it helps with your blood pressure, cholesterol, diabetes, pain, etc your overall health, along with the possibility to stop taking certain medications altogether. Isn't that what Henkel US would prefer!?! He said he didn't know why, I made sense to him what my concern was then stated it was Henkel US who decides my prescription coverage. So who decides Henkel US? Aetna? Caremark? I know it's all about money money to who exactly I don't know.
Who sits in the board room and decides what is really important for the employees, employees spouses, their kids to take preventative measures. To not continue paying the companies share of money.
I would think Henkel US would want this or maybe they don't.
Zero Weight loss medication coverage. Caremark's mission statement: To improve the lives of those we serve by making innovative and high-quality health and pharmacy services safe, affordable and EASY TO ACCESS.
Lie - Only if you are covered, after you go through pre approval which takes 72 hrs if marked urgent, 30 days otherwise. It Is Not Easy.
Wilmington, NC
Caremark repeatedly called me, despite my cell # being marked as ok for text messages only. I had to remove my phone # entirely to make it stop. Their service is sometimes super fast (3-4 days from order to delivery) and sometimes super slow (14+ days, 10+ business days), making it hard to ensure I have a consistent supply of my medications. They make it difficult to update your medication list, which resulted in them harassing one of my doctors for weeks for a medication I was no longer taking. If the alternative wasn't multiple trips to the pharmacy every month I would have quit using them long before now.
I switched insurance to wellcare, they only deal with caremark online. I set up my prescriptions weeks ahead. I go 2 meds late, I still haven't got my insulin after a month. These people are dangerously inept. I have talked to the BBB maybe they can make them do there jobs. Their gonna kill people
Dr called in multiple prescriptions on a tuesday. Called the next Friday because still had not received prescriptions. Was told they would overnight the prescriptions. Called the next Tuesday because still did not receive prescriptions. Caremark said they needed another 3 days to process. Emailed me a USPS tracking number Thursday. As of Saturday USPS tracking stated tracking number created Thursday but USPS had not received package yet. Called Caremark again. Caremark claims it is in transit and delivered Monday. Will call Caremark again Tuesday.

CVS Caremark is by far the worst prescription insurance company.
Prior Authorizations are needed for everything. Females need testosterone too, menopause can start at any age not only 55. They don't cover meds for menopause. They are misogynists.
Customer service is the worst, they need to train the employees in being people.
They told me they won't cover Botox, because it's cosmetic. My neurologist has been helping me with migraines with Botox for years. Express scripts covers this Med, had them for years, but not this joke of a company.

I would give them zero stars if I could. The customer service is HORRIBLE! I have ran out of my prescriptions twice with them both times trying to blame my provider for it when was indeed CVS Caremark's fault not my provider! There is continuously a problem with them and no resolution only excuses and the same problem over and over! Representatives"disconnect" you after being on hold for 30 plus minutes so then you have to call and start over! Soooo frustrating and unprofessional! DO NOT RECOMMEND!

Caremark refuses to order certain prescription drugs stating that their distributor doesn't stock them.
That is a lie. Caremark determines whether a drug should be ordered and what the insurance costs should be.

CVS Caremark is awful. No one should ever have to deal with this. It constitutes abuse to the elderly.

Ordered a prescription refill through their website. They gave me a delivery date, the prescription never arrived. When I called and talked to CSR #1, she told me that my order had been cancelled but couldn't tell me by whom. She promised to get the prescription order resubmitted, and advised me to get a short term supply through my doc. I then received an automated email from CVS Caremark telling me that they were going to delay my prescription refill. I called again, got CSR #2. She tried to blame my physician's office, but then promised to override the system and expedite my refill. The next day, I get another automated message from the system, telling me again that they were delaying the refill. I called CSR # 3 on the phone who then claimed that my prescription had expired, which was not true by CVS Caremark's own record. He went to his supervisor, and after cutting me off called me back to say that CS#2 never filed the override order and they will not expedite the delivery, even though they recognized that I was going to run out of meds again. He told me to go get another short term prescription from my doc and pay it out of pocket. The CVS Caremark reps are powerless to do anything, even when they admit there is a problem. They tell you that they will fix it, and then they don't. Terrible customer service, no self respecting benefits manager who cares about their people should ever sign up with CVS Caremark.

I called these people numerous times for a very important product that is very important. They kept making clerical errors and it is very upsetting.

The insurance company just switched us to CVS Alliance for the "specialty pharmacy" area. Wow, they take incompetence to a new level. I have been calling 5x a day and every time I call it's some new problem. We did the prior authorization last week but suddenly I get a text that we need the prior authorization. Then they are holding up critical meds because of questions about non-critical supplies. It was held up one day because someone on their end made a typo causing a new round of authorizations. I will say: the folks on the phone are super nice. But something is very very very very wrong! Very wrong!

I have Caremark through GEHA. There isn't one medication that I don't pay out of pocket for. They even require a copay for 5mg prednisone-one of the cheapest medications to make. Today, they denied a $50 medication ordered by my physician for a colonoscopy. So, I paid full price. Time to locate a new carrier.

Representative lies, Letter in mail lies, all lies, I called 3 times to verify it was covered medication, NOT covered. Incorrect info given to me. I Paid $253 out of pocket. Shame on CEO
Express Scripts far superior.

Took 8 hours on line to try to prove to CVS Caremark that I did not have another primary insurance company. I still have not resolved the issue. Hours and hours of being transferred from one person to the next. Several promises were made and not followed through. I am a physician and I hope I never have treated a patient as this company has proven not to care. This company should not be in the healthcare industry. Peoples lives are at stake and they have absolutely no cares. Please strike care from Caremark.

I have been purchasing a medication for the past two years at my local CVS pharmacy and paid a total of $10 each time for a 30 day supply. My provider called in the same prescription to CVS Caremark for a 90 day supply which I received a few days later. I didn't think it would matter whether I received the prescription from the store or the mail. Today I get a call from CVS Caremark telling me that I owe them $150 for the 90 day supply. In other words, for a 30 day supply I went from $10 copay in the store to $50 copay online. There is no returning medication so I have no choice but to pay this. I will never use CVS Caremark again. I can see why they are getting poor reviews on this website. Luckily, Walgreens is just as close to me as is my CVS store

I attempted to call CVS Caremark because they would not cover my medication reimbursements stating they had another primary insurance listed for me. It literally took 5 hrs to correct this. This was the second time I had to do this. The first time was in 2021 and it started with the same BS in 2022. I have no other insurance and CVS Caremark is my primary. Then my three prescriptions that they were reimbursing in 2021 were no longer covered in 2021. CVS Caremark offered to fill these for 10 fold more than my local pharmacy and good Rx. I would advise anyone thinking about CVS Caremark as their pharmacy insurance to reconsider. I can see from reading their reviews I Am not alone!
Q&A (3)
What made you choose CVS Caremark over similar businesses?
Answer: Unfortunately, my health insurance provider switched from Express Scripts to CVS Caremark. This would not be my choice!
How easy is it to get a hold of customer service at CVS Caremark?
Answer: I could reach customer service however they do not provide assistance. Unless you request a senior member it's a waist of time.
Have a question?
Ask to get answers from the CVS Caremark staff and other customers.
- Sitejabber’s sole mission is to increase online transparency for buyers and businesses
- Sitejabber has helped over 200M buyers make better purchasing decisions online
- Suspicious reviews are flagged by our algorithms, moderators, and community members
Similar businesses you may also like
See more Pharmacy Businesses- Sitejabber’s sole mission is to increase online transparency for buyers and businesses
- Sitejabber has helped over 200M buyers make better purchasing decisions online
- Suspicious reviews are flagged by our algorithms, moderators, and community members